The Consolidated Appropriations Act, 2021 (CAA) added a new annual reporting requirement for group health plans and health insurance issuers. The new rules require plans to submit an informational report on prescription drug and health care spending to the HHS, the Secretary of Labor, and the Secretary of the Treasury.
The reported information will be aggregated by the departments and published on the internet, with the intention of offering plan sponsors and individuals insight into where their healthcare dollars are spent.
The CMS recently issued detailed reporting instructions that clarify important information about the reporting process for employers.
Which plans are subject?
Essentially all health plans (group and individual) are subject to the new reporting requirements. This includes small and large plans, self-funded and fully insured plans, and both grandfathered and non-grandfathered plans. Essentially, no plans escape this requirement.
Fortunately, the lion’s share of reporting requirements falls on the shoulders of carriers, PBMs, and ASO providers. That said, all employers will be required to file some basic plan data elements.
Which plans are not subject?
The reporting requirement does not apply to health reimbursement accounts (HRAs) and other account-based group health plans (such as FSAs or HRAs). In addition, coverage consisting solely of excepted benefits, such as dental or vision plans, is also exempted.
What data must be included in the reports?
Data required to be included in the reports fall into two categories:
-
Data that is unique to each plan/employer
-
Data that can be aggregated between all plans by a carrier, ASO provider or TPA.
Employer-Specific Data (Non-Aggregated Data)
-
Market segment (large group, small group, etc.)
-
Average number of members covered
-
State in which the plan is offered
-
Average contributions paid by member
-
Average premium paid by employer
-
Total annual premium (or equivalent for self-funded plans)
Plan specific information, such as average contribution, payments by employer, and total premium can be reported by plan or combined for all plans. We believe most employers will find it easier to report the information by health plan.
Aggregated Data
-
50 Most Frequently Dispensed Rx: The 50 brand prescription drugs most frequently dispensed by pharmacies for claims paid by the plan or coverage and the total number of paid claims for each such drug.
-
50 Most Costly Rx: The 50 most costly prescription drugs with respect to the plan or coverage by total annual spending and the annual amount spent by the plan for each such drug.
-
50 Rx with Greatest Cost Increase: The 50 prescription drugs with the greatest increase in plan expenditures over the plan year preceding the plan year that is the subject of the report and, for each such drug, the change in amounts expended by the plan or coverage in each such plan year.
-
Total Plan Spending: Total spending on healthcare services by the plan, broken down by the types of costs, including hospital, primary provider/clinic, specialty provider/clinic, drugs covered by pharmacy benefit, drugs covered by medical benefit, and other costs (such as wellness services).
-
Rx Spend by Spender: Spending on prescription drugs is broken down by the health plan spend and the participant spend (copays and coinsurance).
-
Premium Information: Average monthly premium, including total premium amount, amount paid by plan sponsor, and amount paid by participants. This category applies to total plan premiums, not just the Rx portion.
-
Rebate Information: Prescription drug rebates, fees, and other compensation paid by drug manufacturers to the plan or its administrators or service providers, including the amounts paid for each therapeutic class of drugs, the amounts paid for each of the 25 drugs that yielded the highest amount of rebates, and any reduction in premiums and out-of-pocket costs associated with rebates, fees, or other compensation.
Required Data Elements and Structure
A full report consists of three different elements:
-
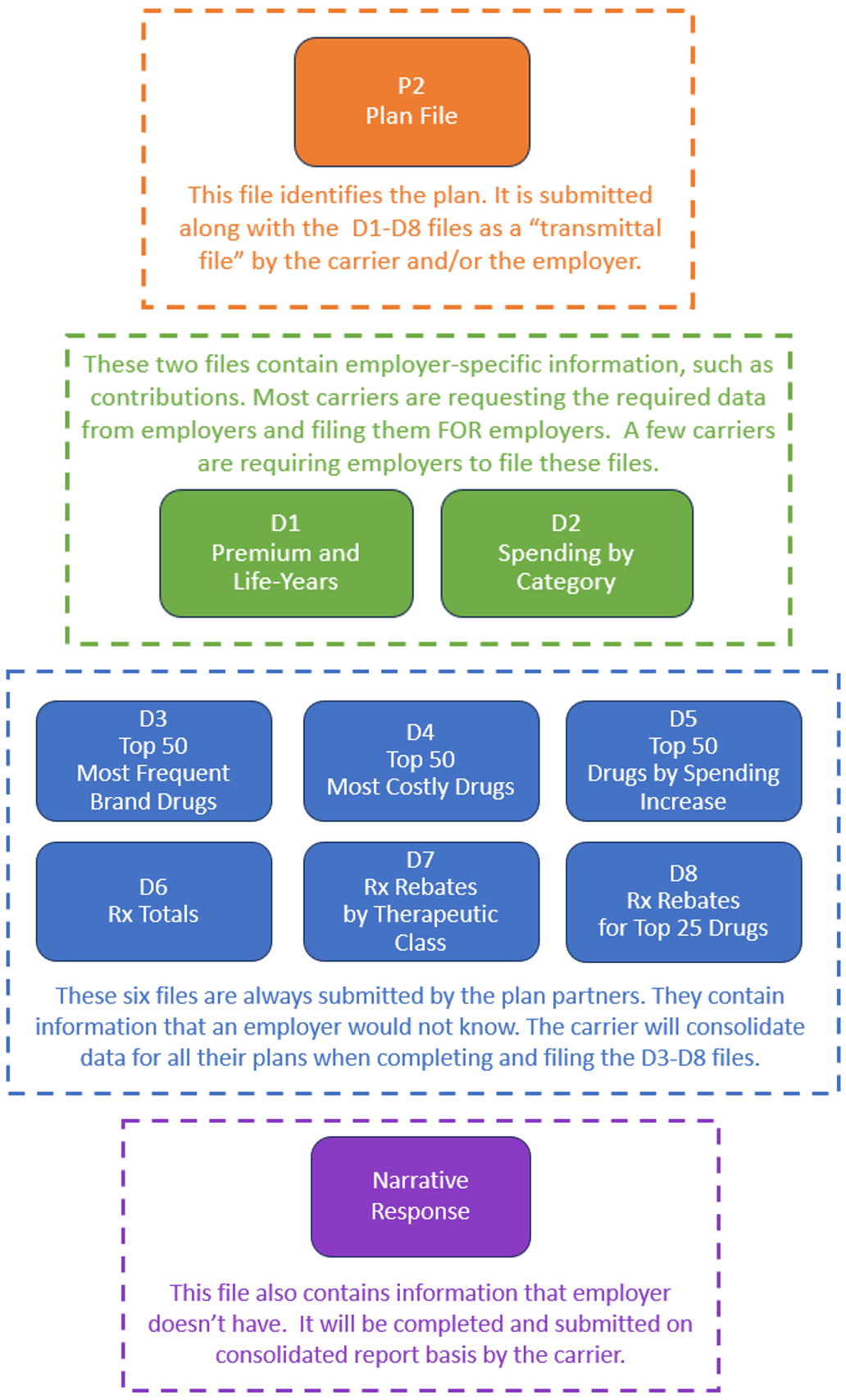
1 Plan File: There are 3 types of Plan files, P1, P2, and P3. The P2 file applies to group health plans. The others don’t apply to employers.
-
8 Data Files: There are 8 required Data files D1, D2, etc. A description of the details for each is outlined below.
-
1 Narrative Response: The Narrative Response must be a pdf or Word file. There are six required elements to address. This will generally be handled by carriers, PBMs, and ASO providers.
The following diagram illustrates what we expect to be a typical division of reporting between employers and plan partners.
Costs for RxDC Reporting
Carriers, TPAs, and PBMs are adopting differing strategies for the RxDC reporting. These entities have and will incur substantial data gathering and reporting costs to comply with the RxDC requirements. As a rule, fully insured carriers have included the cost in overall administration costs and are not charging a direct fee to employers. Some ASO providers, TPAs, and PBMs are passing through a direct fee to employers.
Deadlines for Annual Reports
Reporting runs on a calendar year basis. This law introduced a new term, the “reference year.” The Reference Year is the prior calendar year for which the report is submitted.
Annual reports are due on June 1st following the reference year. June 1, 2024 marks the deadline for the 2023 calendar year.
Employer Action
Employers should keep an eye out for information requests from carriers and other plan partners. Fully insured employers will want to attend to information requests and note the deadline for providing necessary data. Most carriers have set deadlines between March 15th and April 10th.
If you are a Vita Benefits client, your account management team will reach out to you to assist with understanding carrier-imposed deadlines and submission of required information.



